Peripartum Cardiomyopathy and Cesarean Section Report of Two Cases and Literature Review
- Case report
- Open up Access
- Published:
COVID-19 with peripartum cardiomyopathy: a case report
Ain-Shams Periodical of Anesthesiology book 14, Article number:10 (2022) Cite this article
Abstract
Background
The world has been facing the novel coronavirus SARS-CoV-2 pandemic. The novel coronavirus primarily affects the lungs only also affects multiple organ systems including the cardiovascular system causing myocarditis, cardiomyopathy, and arrhythmias. Cardiomyopathy has been reported in patients with COVID-xix; nevertheless, prognosis of peripartum cardiomyopathy in a patient with COVID-xix is still unexplored. More than knowledge is required to sympathize the incidence of cardiomyopathy due to novel coronavirus SARS-CoV-2.
Case presentation
We report a instance of peripartum cardiomyopathy gravida 2 parity 2 COVID-19 confirmed patient who underwent an emergency preterm lower segment caesarean section (LSCS) for astringent pre-eclampsia and intra-uterine growth retardation (IUGR) and landed upward in astute congestive cardiac failure with pulmonary oedema. A postpartum 32 years female presented to our found, a dedicated COVID-19 hospital with tachycardia, hypertension, anasarca, tachypnea with desaturation on room air. She had undergone emergency caesarean section for severe preeclampsia with intrauterine growth retardation. On post-operative day ii (POD2), she complained of shortness of breath. On POD iii she tested positive RT-PCR for COVID-19 infection. She responded to treatment with steroids. All the same, on POD6, She developed severe pulmonary oedema with poor ejection fraction necessitating endotracheal intubation and pressure control ventilation. Congestive cardiac failure was managed with diuretics and digoxin. Gradually oxygenation improved. She was electively ventilated for 3 days. Gradually, ejection fraction improved with the resolution of B lines. On the ninth POD, after a successful spontaneous breathing trial, she was extubated and not-invasive ventilation with bi-level positive airway pressure was fastened. The patient was gradually tapered off of the non-invasive ventilation over 2 days. On the 11th post-operative 24-hour interval, she was maintaining oxygen saturation on nasal prongs and was sent to the ward.
Conclusions
We recommend early employ of bedside lung ultrasonography; echocardiography and shut cardiovascular monitoring in severe COVID-19 infected pregnant patients who present with shortness of breath, tachypnea, and hypertensive disorders of pregnancy and previous cardiac abnormalities for expedite management and improved prognosis. An platonic case scenario for extubation may not exist nowadays, not-invasive ventilation with bi-level positive airway pressure level mail service-extubation helps in patients with peripartum cardiomyopathy.
Background
The electric current novel coronavirus SARS-CoV-2 pandemic has affected millions of people worldwide and numbers are continuously increasing. It is a deadly virus particularly mortiferous in the vulnerable and high-risk population. Such a high-risk grouping is significant females. Physiological changes in pregnancy such every bit reduced functional residual volume, contradistinct cell immunity, and elevation of diaphragm increment the susceptibility of contracting COVID-nineteen infection. Nosotros are in a continuous state of learning nigh the COVID-19 disease its pathophysiology, complications and management. Cardiomyopathy in pregnant and non-pregnant patients is 1 such dreaded complication reported due to SARS-CoV-two infection which can be proved fatal if non diagnosed during the early stages. Peripartum cardiomyopathy presents with typical signs and symptoms of astute congestive eye failure and symptoms may mimic physiological changes of pregnancy thus echocardiography helps confirm the diagnosis. Once diagnosed, management includes non-invasive or invasive ventilatory support, the establish's standard protocol for the handling of COVID-19, classical treatment goals of eye failure, and should include thromboembolic prophylaxis. Here we present a case where a gravida 2 para ii confirmed case of COVID-xix underwent emergency preterm lower segment caesarean section (LSCS) for severe pre-eclampsia and intra-uterine growth retardation (IUGR) and landed up in acute congestive middle failure with pulmonary oedema and its successful direction.
Case presentation
A postpartum32years female presented to our institute, a dedicated COVID-19 hospital with tachycardia (heart rate of 110 bpm), hypertension (BP 180/110 mmHg), anasarca, tachypnea with desaturation on room air (SpOii 84%). She had undergone emergency caesarean section for severe preeclampsia with intrauterine growth retardation at thirty weeks of gestation nether regional anaesthesia three days back. She was transfused 1 unit of packed red claret cells on the showtime postoperative twenty-four hour period (POD1). All the same, on POD2 she complained of shortness of breath with uneasiness and was managed with oxygen supplementation and Pritchard regime for the control of preeclampsia. By Pritchard regimen, a loading dose of four chiliad of twenty% magnesium sulphate 4 was given, immediately followed by 10 yard of 50% magnesium sulphate intramuscularly (five thousand in each buttock) and maintenance dose 5 g of 50% MgSO4 IM iv hourly in alternate buttocks for 24 h.
When there was no improvement, she was referred to our institute with suspicion of COVID-19 infection. The patient had no known contact with COVID-19 cases and had no travelling history. She is a known hypothyroid on tablet levo-thyroxine 50 μg once a twenty-four hour period. There was no significant medical, family, psycho-social history, and surgical history.
She was initially managed for hypertensive crunch with astringent preeclampsia with supplemental oxygen with loftier catamenia nasal cannula, tablet torsemide ten mg 12 hourly, infusion labetalol at x mg/h, and magnesium sulphate for 24 h for seizure prophylaxis along with antibiotics and levothyroxine fifty μg OD equally she was a known hypothyroid patient. All the same, with a positive RT-PCR for COVID infection, she was further given dexamethasone eight mg 12 hourly for cytokine storm and therapeutic dose of subcutaneous enoxaparin 60 mg BD with Tab ecosprin 75 mg OD to prevent thromboembolic complications. Intendance was taken to avoid whatsoever further source of sepsis and intramuscular injections. She responded to treatment with decrease in oedema, controlled blood pressure level, and saturation of 97% on room air and was shifted to the ward later ii days of ascertainment.
However, on the 6th postoperative 24-hour interval, she developed obtundation, severe pulmonary oedema (B-lines on USG Lung) with poor ejection fraction necessitating endotracheal intubation and pressure level control ventilation with inspiratory force per unit area back up (PS) of 22 mmHg and positive end-expiratory pressure (PEEP) of 10 with fraction of inspired oxygen (FiO2) one.0. Her oxygen saturation remained 85–90% for the next hour (Table 1). Lung ultrasonography revealed bilateral B-lines, with poor left ventricular ejection fraction of 30%. She was diagnosed with acute congestive cardiac failure (CCF) with COVID pneumonia (Fig. 1). Management of CCF was done with furosemide infusion (20 mg/h) and intravenous digoxin 0.125 mg 12 hourly. Gradually oxygenation improved with FiO2 requirement decreased to 0.6. Antibiotics were empirically upgraded to meropenem with teicoplanin. A catheter was inserted in the right internal jugular vein for giving ionotopes, vasodilators, drugs, and to take access to claret samples. Arterial cannula was inserted in the correct radial artery for the beat to beat claret pressure monitoring and drawing sample for arterial blood gas analysis. However, the next twenty-four hour period, in view of hypokalaemia, digoxin was withheld with the initiation of nitroglycerine infusion (1 μg/kg/min), dobutamine infusion (5 μg/kg/min) and correction of hypokalaemia (Table ii). She was electively ventilated for three days. Gradually, ejection fraction improved to 50% with resolution of B lines and improvement in oxygenation. On the 9th POD, after a successful spontaneous breathing trial on pressure level support of 10 mmHg, PEEP v mmHg, the trachea was extubated and non-invasive ventilation with bi-level positive airway force per unit area (BiPAP) attached with the same settings (Fig. 2). Immediately mail-extubation, nitroglycerine infusion was gradually tapered off. Tablet carvedilol 3.125 mg OD and ramipril 2.v mg BD were started to decrease afterload and better left ventricular ejection fraction with continuation of diuretics (furosemide 20 mg IV viii hourly) to subtract preload. On the 11th post-operative twenty-four hours, she was maintaining oxygen saturation 97–98% on nasal cannula at two L/min and was sent to the ward. The baby of the patient has tested negative for RT-PCR for COVID-nineteen infection.
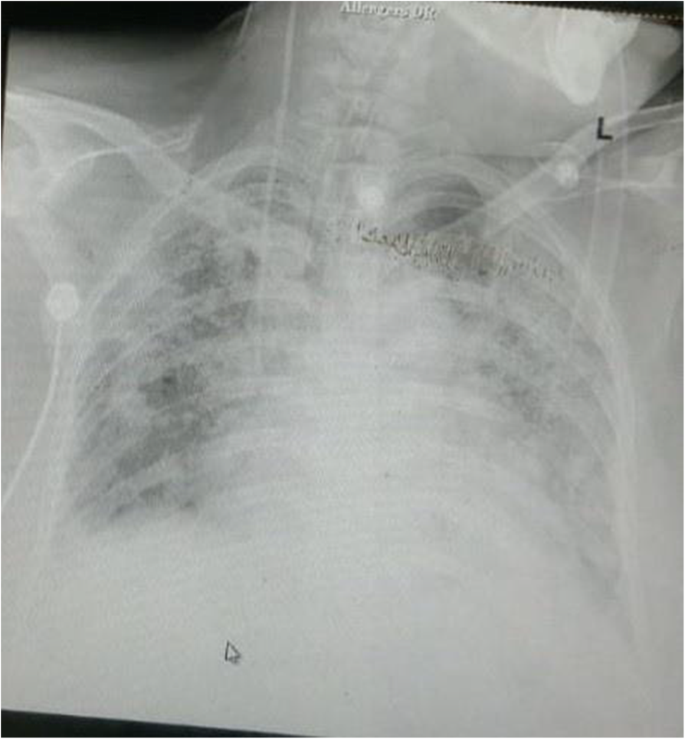
Chest Ten-ray on POD6 showing astute congestive cardiac failure with ARDS

Chest Ten-ray on POD9
The patient has been asked to follow up in the cardiology outpatient section later half dozen months. At the fourth dimension of submission of this example report, the patient has been discharged to home afterwards testing negative for RT-PCR for COVID-xix infection. The patient was satisfied with the handling and was very thankful to all the doctors, nursing staff and all the staff involved in her treatment.
Discussion
SARS-CoV-2 is non but a respiratory virus, but it has multi-organ affinity (Spuntarelli et al., 2020)..Cardiomyopathy has an incidence of 33% in critically ill non-pregnant patients with COVID-19 (Guo et al., 2020). Various mechanisms proposed include increased inflammatory response, downregulation of angiotensin-converting enzyme two receptors, autonomic tone disturbance, increased endogenous catecholamines, hypercoagulable state, hypoxaemia, cardiopulmonary deconditioning, and peripheral deconditioning. All these lead to myocardial injury and conduction arrangement damage which leads to hypotension, decompensated heart failure, astute coronary syndrome, tachyarrhythmia, bradyarrhythmia, and sudden cardiac death (Kochi et al., 2020).
A recently published case series described two cases of COVID-19–related cardiomyopathy in the pregnant patient. However, both of these patients possessed multiple risk factors for cardiac disease, and information technology remained unclear equally to whether cardiomyopathy occurred as a direct complication of COVID-19, or secondary to multiorgan dysfunction (Juusela et al., 2020). Dilemma of diagnosis remains between peripartum cardiomyopathy (PPCM) and COVID-xix-related cardiomyopathy.
In our patient, the differential diagnoses made were PPCM, hypertensive congestive cardiac failure due to severe preeclampsia, COVID-19-related cardiomyopathy, or myocarditis due to other cardiotropic viruses. PPCM is a rare acute life-threatening complication of pregnancy, is a class of dilated cardiomyopathy divers by left ventricular systolic dysfunction and cardiac failure in the final month of pregnancy or inside 5 months of commitment, absence of previous heart disease, and absence of identifiable causes of cardiac failure. Echocardiogram in our patient showed moderate to severe left ventricular systolic harm with an ejection fraction 35–40%. The left atrium and valves were normal. The structural changes within the myocardium secondary to hypertension causing dumb myocardial relaxation resulting in diastolic failure were absent in our example. The patient was found negative for the screen of cardiotropic viruses.
Our constitute is a dedicated COVID facility. It provides free of price investigations and handling for COVID positive patients. With logistic issues and limited resources in face of the overwhelming COVID-xix pandemic, nosotros were unable to get patient's, series cardiac biomarkers, cardiac magnetic resonance imaging, cardiac biopsy, high resolution computed tomography browse breast to found COVID-19 as the direct crusade of cardiomyopathy. Arcari et al. in their study have found that the cardiac biomarkers top was common in COVID-19 pneumonia and is associated with worse prognosis (Arcari et al., 2020). However, every bit per the disease course, the aetiology of cardiac failure in our patient is likely to have been a congestive cardiac failure with pulmonary oedema due to peripartum cardiomyopathy which may have been exacerbated by COVID-nineteen.
The management of all peripartum cardiomyopathy is multimodal with diuretics, digoxin, dobutamine and nitroglycerine to decrease preload, improve cardiac contractility and decrease afterload. Hence, in the setting of COVID-nineteen, some other crucial attribute becomes the management of the inflammatory response and prevention of thromboembolic complications. We were able to manage the inflammatory response with dexamethasone eight mg IV BD with therapeutic dose of enoxaparin. An ideal extubation scenario may not exist available in patients with COVID-19. It is imperative to avoid iatrogenic ventilator-associated pneumonia. We extubated our patient after 48 h with a force per unit area support requirement of ten mm Hg, PEEP 5 mmHg, and supplemented with BiPAP which was tolerated well past the patient.
Conclusions
Due to lack of data on COVID-19 infected meaning patients and cardiomyopathy, further studies on pregnant patients infected with COVID-19 are required. Ethical dilemma rules out any prospective or randomized controlled studies. Till the time such data is available, every case report may contribute to further learning in this vulnerable group of population if inflicted with COVID-19. We recommend echocardiography and close cardiovascular monitoring in severe COVID-19 infected pregnant patients who presents with respiratory distress and preeclampsia for timely management and prevention of fatal outcome. Direction of COVID-xix inflammatory state should get alongside treatment of cardiac failure. Early extubation may reduce iatrogenic ventilator-induced injury.
Availability of data and materials
Not applicable
Abbreviations
- LSCS:
-
Lower segment caesarean section
- IUGR:
-
Intra-uterine growth retardation
- CCF:
-
Congestive cardiac failure
- PPCM:
-
Peripartum cardiomyopathy
- POD:
-
Post-operative mean solar day
- PEEP:
-
Positive end-expiratory pressure
- BiPAP:
-
Bi-level positive airway force per unit area
References
-
Arcari L, Luciani M, Cacciotti L, Musumeci MB, Spuntarelli V, Pistella E, Martolini D, Manzo D, Pucci One thousand, Marone C, Melandri S, Ansalone Thousand, Santini C, Martelletti P, Volpe M, De Biase 50 (2020) Incidence and determinants of high-sensitivity troponin and natriuretic peptides summit at admission in hospitalized COVID-nineteen pneumonia patients. Intern Emerg Med xv(eight):1467–1476. https://doi.org/10.1007/s11739-020-02498-vii
-
Guo T, Fan Y, Chen Thou (2020) Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol five(7):811–818. https://doi.org/10.1001/jamacardio.2020.1017
-
Juusela A, Nazir M, Gimovsky One thousand (2020) Two cases of coronavirus 2019 related cardiomyopathy in pregnancy. Am J Obstet Gynecol MFM 2(ii):100113. https://doi.org/10.1016/j.ajogmf.2020.100113
-
Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C (2020) Cardiac and arrhythmic complications in patients with COVID-nineteen. J Cardiovasc Electrophysiol 31(5):1003–1008. https://doi.org/10.1111/jce.14479
-
Spuntarelli V, Luciani Thousand, Bentivegna East, Marini Five, Falangone F, Conforti M, Rachele ES, Martelletti P (2020) COVID-19: is it just a lung disease? A instance-based review. SN Compr Clin Med:1–6. https://doi.org/10.1007/s42399-020-00418-six
Writer information
Affiliations
Contributions
PT, STK and PS are a team of anaesthesiologists involved in the treatment of the patient mentioned in the instance report. PT is tmajor contributor in writing the manuscript under the guidance of STK and PS. All authors have read and approved the final manuscript.
Respective author
Ethics declarations
Ideals approval and consent to participate
Ideals approval and written informed consent for participation was obtained from the guardian of the patient. A copy of the consent form is available for review by the Editor of this periodical.
Consent for publication
Written informed consent for publication of the clinical details and /or clinical images was obtained from the guardian of the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Boosted data
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Admission This article is licensed nether a Creative Commons Attribution iv.0 International License, which permits employ, sharing, adaptation, distribution and reproduction in whatever medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Eatables licence, and bespeak if changes were made. The images or other third party textile in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the textile. If cloth is not included in the commodity's Creative Eatables licence and your intended use is not permitted by statutory regulation or exceeds the permitted apply, y'all will need to obtain permission direct from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/four.0/.
Reprints and Permissions
Near this article
Cite this article
Karna, Southward.T., Thaware, P. & Singh, P. COVID-19 with peripartum cardiomyopathy: a case report. Ain-Shams J Anesthesiol fourteen, ten (2022). https://doi.org/10.1186/s42077-021-00204-z
-
Received:
-
Accustomed:
-
Published:
-
DOI : https://doi.org/ten.1186/s42077-021-00204-z
Keywords
- COVID-xix
- Cardiomyopathy
- Congestive cardiac failure
- Echocardiography
Source: https://asja.springeropen.com/articles/10.1186/s42077-021-00204-z
0 Response to "Peripartum Cardiomyopathy and Cesarean Section Report of Two Cases and Literature Review"
Post a Comment